The Ultimate Guide for Nurses: Enhancing Communication with Chronic Pain Patients
Have you ever felt frustrated because your patients with chronic pain just don’t seem to understand their treatment plan? Improving chronic pain patient communication is crucial for effective care.
As a life coach, I’ve seen how improving communication can transform patient outcomes. In my experience, effective communication is key in managing chronic pain. This includes utilizing empathetic listening skills for nurses and implementing effective pain assessment techniques.
In this article, you’ll learn actionable strategies to enhance your communication skills with chronic pain patients. We’ll cover personalized management plans, using visual aids, and more. These strategies will help in building trust with chronic pain patients and improving overall care.
Let’s dive in to explore ways of improving chronic pain patient communication and enhancing patient education on pain management.

Understanding Communication Challenges in Chronic Pain Management
Improving chronic pain patient communication is often one of the biggest hurdles in chronic pain management. In my experience, many nurses struggle to convey treatment plans and understand patient concerns, leading to frustration for both parties. Effective pain assessment techniques and empathetic listening skills for nurses are crucial in this process.
When communication breaks down, patients may feel misunderstood and neglected. This can significantly impact their satisfaction and adherence to treatment plans. Patient education on pain management and culturally competent pain communication are key factors in improving chronic pain patient communication.
I’ve seen several clients report that inconsistent communication leaves them feeling more anxious and less confident in their care. Building trust with chronic pain patients is essential for effective pain management.
Professional nursing organizations frequently highlight these gaps. They emphasize the need for improved communication strategies to ensure better patient outcomes. Interdisciplinary collaboration in chronic pain care and pain scale utilization and interpretation are important aspects of improving chronic pain patient communication.
Addressing these challenges is crucial for enhancing the overall quality of care and patient satisfaction. Non-pharmacological pain management strategies and motivational interviewing for chronic pain patients can contribute to more effective communication and improved outcomes.

Key Steps to Enhance Communication with Chronic Pain Patients
Improving chronic pain patient communication requires a few key steps. Here are the main areas to focus on to make progress.
- Develop individualized pain management plans: Tailor plans to each patient’s unique needs, incorporating effective pain assessment techniques.
- Utilize visual aids to explain pain concepts: Use diagrams and digital tools to illustrate pain pathways and treatments, aiding in patient education on pain management.
- Practice active listening during patient encounters: Allocate time for patients to share their experiences without interruptions, enhancing empathetic listening skills for nurses.
- Incorporate cultural competence in assessments: Enhance understanding of diverse backgrounds through training, focusing on culturally competent pain communication.
- Educate on non-pharmacological pain strategies: Provide resources on Cognitive Behavioral Therapy and mindfulness as non-pharmacological pain management strategies.
- Involve family members in care discussions: Engage families in appointments and education, promoting interdisciplinary collaboration in chronic pain care.
- Implement regular pain communication training: Schedule training sessions to improve communication techniques, including pain scale utilization and interpretation.
Let’s dive in to further explore these steps for improving chronic pain patient communication!
1: Develop individualized pain management plans
Creating personalized pain management plans is essential for effectively addressing each patient’s unique needs and concerns, improving chronic pain patient communication.
Actionable Steps:
- Assess each patient’s pain experience and history using effective pain assessment techniques to tailor their management plan.
- Set SMART goals for pain management with patients, ensuring they are specific, measurable, actionable, realistic, and time-bound.
- Regularly review and adjust pain management plans based on patient feedback and progress, utilizing empathetic listening skills for nurses.
Explanation:
Personalized pain management plans are crucial because they address the specific challenges and preferences of each patient. This individualized approach can significantly enhance patient satisfaction and treatment outcomes, including non-pharmacological pain management strategies.
According to the Whole Health Library, understanding and adapting to each patient’s pain experience is key to effective care.
When you tailor pain management plans, you help build trust with chronic pain patients and improve communication. This personalized care not only leads to better pain management but also enhances overall patient well-being through patient education on pain management.
Key benefits of personalized pain management plans include:
- Improved patient adherence to treatment
- Enhanced patient-provider communication, including culturally competent pain communication
- Better long-term pain management outcomes through interdisciplinary collaboration in chronic pain care
Next, let’s explore how visual aids can enhance understanding.

2: Utilize visual aids to explain pain concepts
Utilizing visual aids can significantly enhance patient understanding and retention of pain management information, which is crucial for improving chronic pain patient communication.
Actionable Steps:
- Create and use diagrams or charts to illustrate pain pathways and management techniques, including non-pharmacological pain management strategies.
- Implement digital tools or apps that provide visual explanations of pain and treatment options, enhancing effective pain assessment techniques.
- Use visual aids during patient education on pain management sessions to reinforce understanding and retention.
Explanation:
Visual aids are crucial because they make complex pain concepts more accessible and easier to grasp. By utilizing visual tools, you ensure that patients can visualize their pain pathways and understand treatment options better, improving chronic pain patient communication.
According to the Wolters Kluwer, visual aids effectively reinforce learning and improve patient comprehension, which is essential for building trust with chronic pain patients.
Next, let’s explore the importance of practicing active listening during patient encounters, a key component of empathetic listening skills for nurses.

3: Practice active listening during patient encounters
Active listening is crucial in improving chronic pain patient communication and addressing their needs effectively.
Actionable Steps:
- Allocate dedicated time for each patient to share their pain experiences without interruptions, enhancing effective pain assessment techniques.
- Reflect back what the patient has said to ensure understanding and validation, demonstrating empathetic listening skills for nurses.
- Encourage patients to ask questions and express concerns, and respond empathetically and thoroughly, building trust with chronic pain patients.
Explanation:
These steps matter because active listening fosters trust and opens up better communication channels for improving chronic pain patient communication. This practice helps nurses understand patient concerns more deeply and respond more effectively, supporting non-pharmacological pain management strategies.
According to the Whole Health Library, listening attentively to patients’ pain experiences is key to effective care and accurate documentation of patient pain experiences.
Next, let’s explore the importance of incorporating cultural competence in assessments, focusing on culturally competent pain communication.

4: Incorporate cultural competence in assessments
Incorporating cultural competence in assessments is essential to provide effective and personalized care to diverse patient populations, especially when improving chronic pain patient communication.
Actionable Steps:
- Attend cultural competence workshops or training sessions to enhance understanding of diverse patient backgrounds and develop culturally competent pain communication skills.
- Use culturally sensitive assessment tools to evaluate pain and its impact on different populations, ensuring effective pain assessment techniques.
- Collaborate with cultural liaisons or patient advocates to ensure culturally appropriate care and foster interdisciplinary collaboration in chronic pain care.
Explanation:
These steps matter because understanding cultural differences can significantly improve patient trust and communication. This approach ensures that care is tailored to individual needs and backgrounds, enhancing chronic pain patient communication.
According to the OpenStax Clinical Nursing Skills, cultural competence in pain assessment and management is crucial for effective care.
Key aspects of cultural competence in pain management:
- Recognizing cultural differences in pain expression
- Adapting communication styles to patient preferences, utilizing empathetic listening skills for nurses
- Understanding cultural beliefs about pain and treatment, including non-pharmacological pain management strategies
Next, let’s explore the importance of educating on non-pharmacological pain strategies.

5: Educate on non-pharmacological pain strategies
Educating patients on non-pharmacological pain strategies is essential for improving chronic pain patient communication and comprehensive pain management.
Actionable Steps:
- Provide resources and training on techniques like Cognitive Behavioral Therapy (CBT), mindfulness, and relaxation exercises as part of non-pharmacological pain management strategies.
- Organize group sessions or workshops on non-pharmacological pain management methods to enhance patient education on pain management.
- Follow up with patients to monitor their use of these strategies and offer additional support as needed, utilizing empathetic listening skills for nurses.
Explanation:
These steps matter because non-pharmacological strategies can enhance pain management without the risks associated with medication, contributing to effective pain assessment techniques.
Techniques like CBT and mindfulness can significantly improve patient outcomes and are crucial for improving chronic pain patient communication.
According to the Whole Health Library, educating patients on these methods is crucial for holistic care and building trust with chronic pain patients.
Next, let’s explore the importance of involving family members in care discussions as part of interdisciplinary collaboration in chronic pain care.

6: Involve family members in care discussions
Involving family members in care discussions is crucial for improving chronic pain patient communication and comprehensive management.
Actionable Steps:
- Invite family members to patient appointments to discuss pain management plans and strategies, including effective pain assessment techniques.
- Provide educational materials and resources for family members to support the patient’s pain management at home, emphasizing non-pharmacological pain management strategies.
- Encourage family involvement in setting and achieving pain management goals, utilizing empathetic listening skills for nurses.
Explanation:
These steps matter because family support can significantly enhance patient adherence to pain management plans and improve overall outcomes in chronic pain care.
Engaging family members in care discussions fosters a supportive environment and ensures that patients receive consistent support at home, which is essential for building trust with chronic pain patients.
According to the CDC, patient engagement and communication are essential in the diagnostic process.
Now, let’s explore the importance of regular pain communication training.

7: Implement regular pain communication training
Regular pain communication training is vital to ensure nurses stay updated on the best practices for improving chronic pain patient communication.
Actionable Steps:
- Schedule monthly training sessions focused on effective pain assessment techniques and communication strategies specific to chronic pain management.
- Create a mentorship program where experienced nurses can guide and support newer staff in developing empathetic listening skills for nurses and effective communication practices.
- Use role-playing exercises to practice and refine communication skills in various pain management scenarios, including culturally competent pain communication.
Explanation:
These steps matter because continuous training enhances communication skills, leading to better patient outcomes. A mentorship program fosters a culture of shared knowledge and support, promoting interdisciplinary collaboration in chronic pain care.
According to the Wolters Kluwer, regular training and mentorship are key to effective patient education on pain management.
Benefits of regular pain communication training:
- Improved patient satisfaction and outcomes through effective pain scale utilization and interpretation
- Enhanced team collaboration and knowledge sharing on non-pharmacological pain management strategies
- Reduced risk of miscommunication and errors when documenting patient pain experiences accurately
By implementing these practices, you can ensure that your team is always prepared to communicate effectively with chronic pain patients, utilizing motivational interviewing techniques and building trust with chronic pain patients.

Partner with Alleo to Improve Chronic Pain Communication
We’ve explored the challenges of improving chronic pain patient communication and the steps to achieve it. Did you know you can work directly with Alleo to make this journey easier and faster?
Setting up an account with Alleo is simple. Create a personalized plan to enhance your communication skills, including effective pain assessment techniques and empathetic listening skills for nurses.
Alleo’s AI coach provides tailored coaching support, just like a human coach. The coach will follow up on your progress, handle changes, and keep you accountable via text and push notifications. This approach helps in building trust with chronic pain patients and supports interdisciplinary collaboration in chronic pain care.
Ready to get started for free? Let me show you how to improve your skills in documenting patient pain experiences accurately and utilizing pain scale interpretation!
Step 1: Logging in or Creating an Account
To begin improving your communication with chronic pain patients, log in to your existing Alleo account or create a new one to access personalized coaching and support.

Step 2: Choose Your Focus Area
Click on “Building better habits and routines” to start improving your communication skills with chronic pain patients. This focus area will help you develop consistent practices for effective patient interactions, enhancing your ability to provide personalized care and support.

Step 3: Select “Health” as Your Focus Area
Choose “Health” as your primary focus area in the Alleo app to address chronic pain management and improve patient communication, aligning perfectly with your goal of enhancing healthcare outcomes.

Step 4: Starting a Coaching Session
Begin your journey with Alleo by scheduling an intake session, where you’ll discuss your communication challenges with chronic pain patients and create a personalized plan to enhance your skills.

Step 5: Viewing and managing goals after the session
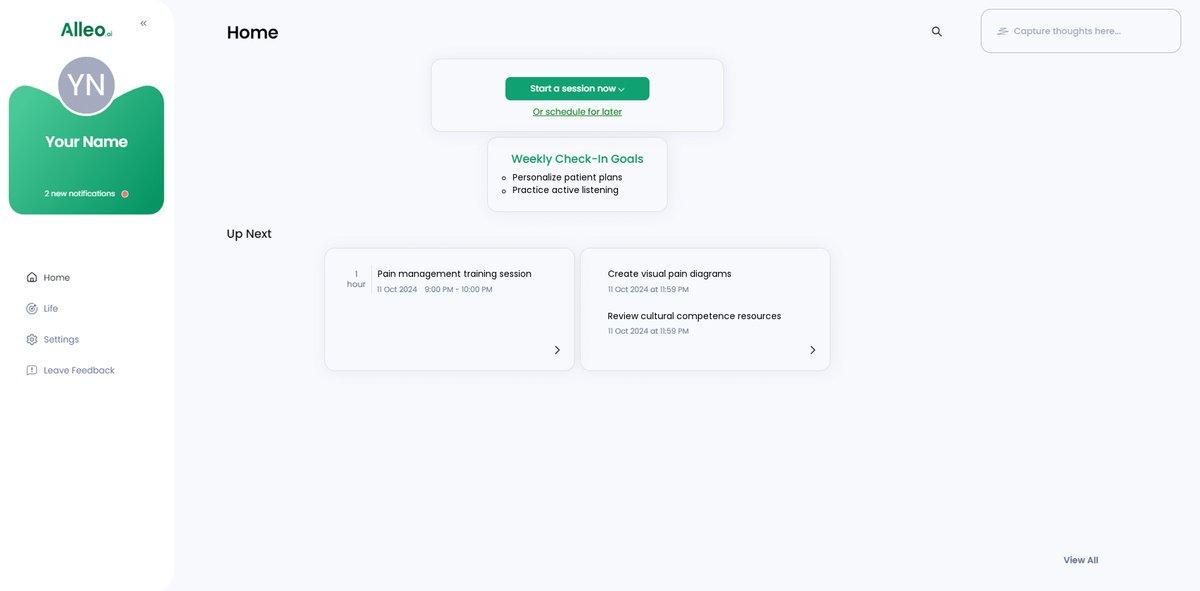
After your coaching session on improving communication with chronic pain patients, you’ll find your personalized goals displayed on the home page of the Alleo app, making it easy to review and track your progress in enhancing patient care.
Step 6: Adding events to your calendar or app
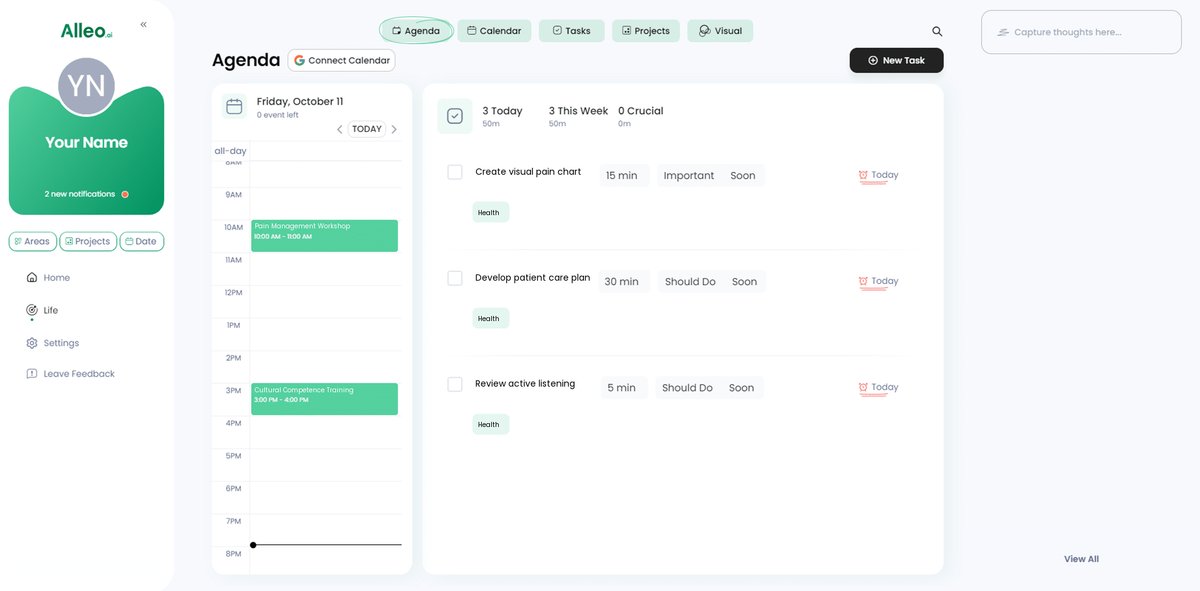
Use the calendar and task features in the Alleo app to schedule and track your progress on communication improvement activities, such as patient education sessions or family care discussions, ensuring you stay on top of your chronic pain management goals.
Bringing It All Together for Better Patient Communication
Improving chronic pain patient communication is challenging but crucial. You have the power to make a real difference.
By implementing personalized plans, using visual aids, and practicing empathetic listening skills for nurses, you can transform patient experiences. Remember, culturally competent pain communication and non-pharmacological pain management strategies are key to holistic care.
Involving family members and consistent training in effective pain assessment techniques will further enhance your effectiveness. These steps may seem small, but they add up to significant improvements in improving chronic pain patient communication.
Let’s not forget, Alleo is here to help. Our platform makes it easier to apply these strategies and track your progress in documenting patient pain experiences accurately.
Start your journey with Alleo today. Your patients will thank you for building trust with chronic pain patients.